Introduction
In the field of dentistry, dental emergencies can present ethical dilemmas that require careful decision-making. Dentists often find themselves facing challenging situations where they must balance the immediate needs of the patient with ethical considerations. This article explores the ethical decision-making process in dental emergencies and provides insights into how dentists can navigate these dilemmas.
Understanding Ethical Decision-Making
Ethical decision-making involves evaluating the potential consequences of different actions and choosing the course of action that aligns with ethical principles. In dental emergencies, dentists must consider the well-being of the patient, the available resources, and the ethical guidelines set by professional organizations.
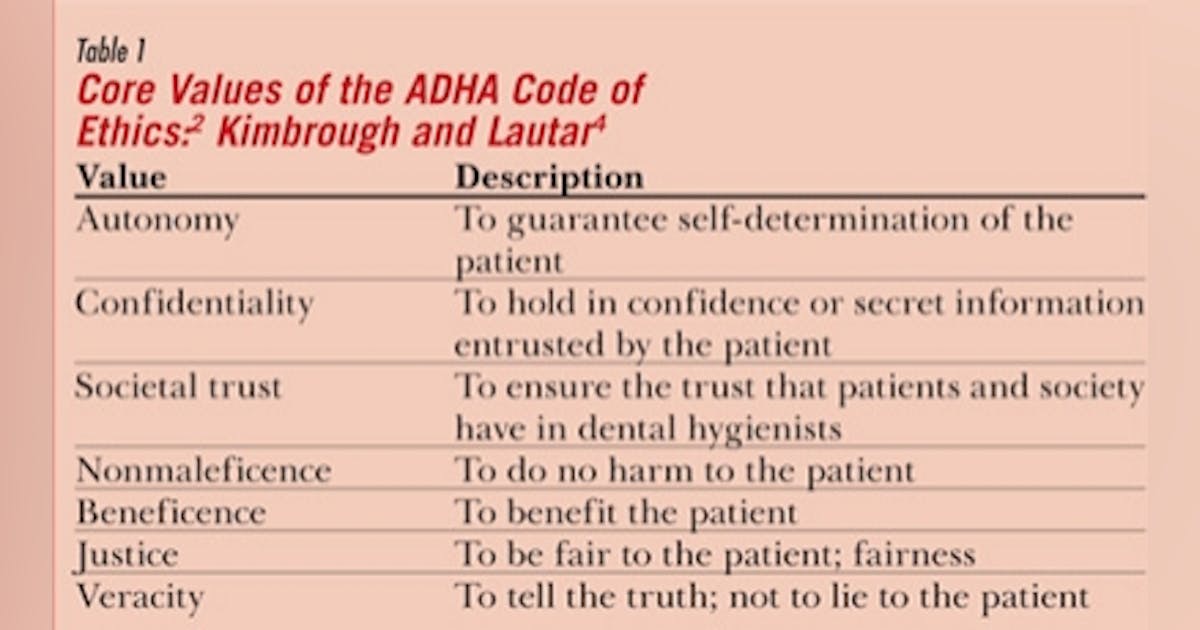
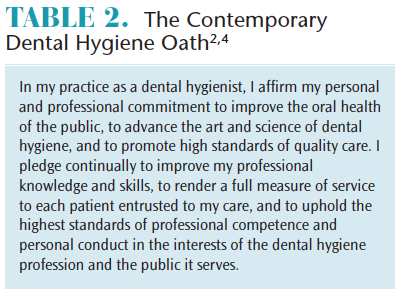
Ethical Principles in Dentistry
Dentistry is guided by several ethical principles, including beneficence (doing good), non-maleficence (avoiding harm), autonomy (respecting patient’s choices), and justice (fair distribution of resources). Dentists must uphold these principles while making decisions in dental emergencies.
Assessing the Situation
When faced with a dental emergency, dentists must first assess the situation to determine the severity and urgency of the problem. This assessment helps in prioritizing the patient’s needs and allocating resources effectively.
Triaging Patients
Triaging involves categorizing patients based on the severity of their condition. Dentists must use their professional judgment to determine who requires immediate attention and who can wait. This process ensures that patients with life-threatening emergencies receive prompt care.
Informed Consent
Obtaining informed consent is crucial in dental emergencies. Dentists must communicate the risks, benefits, and alternatives of the proposed treatment to the patient or their legal guardian. In emergency situations, obtaining consent may be challenging, but dentists should make every effort to involve the patient or their representative in the decision-making process.
Proxy Decision-Making
In cases where the patient is unable to provide consent, dentists may need to rely on proxy decision-makers, such as family members or legal guardians. Dentists should follow legal and ethical guidelines.
Summary
Dealing with dental emergencies involves more than just providing immediate care. Dental professionals must also consider the ethical implications of their decisions. This blog post will delve into the various ethical dilemmas that can arise in dental emergencies, such as prioritizing treatment, managing patient expectations, and ensuring informed consent. We will explore the ethical principles that guide decision-making in these situations, including beneficence, non-maleficence, autonomy, and justice. Additionally, we will discuss strategies to help dental professionals navigate these dilemmas, such as effective communication, collaboration with colleagues, and seeking guidance from professional organizations. By understanding the importance of ethical decision-ma find here king and implementing appropriate strategies, dental professionals can ensure the best possible outcomes for their patients in dental emergencies.
- Q: What should I do if a patient with a dental emergency cannot afford the necessary treatment?
A: Dentists have a professional obligation to provide emergency care to patients in need, regardless of their ability to pay. You can explore alternative treatment options, such as temporary solutions or referring the patient to a dental clinic that offers reduced-cost or free services. - Q: How should I handle a situation where a patient refuses recommended treatment for a dental emergency?
A: It is important to respect a patient’s autonomy and right to make decisions about their own healthcare. Engage in open and honest communication to understand their concerns or reasons for refusal. Provide them with all the necessary information about the risks and consequences of not receiving the recommended treatment. If they still refuse, document the discussion and have them sign a refusal of treatment form. - Q: What should I do if I suspect a case of dental abuse or neglect?
A: If you suspect dental abuse or neglect, it is your ethical duty to report it to the appropriate authorities, such as child protective services or adult protective services. Document any observations or evidence that supports your suspicion and follow the reporting procedures mandated by your jurisdiction. - Q: How should I handle a situation where a patient requests a procedure that is unnecessary or potentially harmful?
A: As a dentist, you have a responsibility to prioritize the well-being of your patients. Engage in a thorough discussion with the patient to understand their motivations and concerns. Provide them with evidence-based information about the risks and benefits of the requested procedure. If you believe the procedure is unnecessary or harmful, it is your ethical duty to explain your professional opinion and recommend alternative treatments or seek a second opinion if necessary. - Q: What should I do if I make a mistake during a dental emergency procedure?
A: Mistakes can happen, even in emergency situations. The most important thing is to prioritize patient safety and well-being. Immediately inform the patient about the mistake, apologize sincerely, and take appropriate steps to rectify the situation. This may involve seeking assistance from a more experienced colleague, providing additional treatment, or referring
Welcome to my website! My name is Cameron Nicoll, and I am a dedicated and passionate Dental Lab Technician with a strong focus on Clear Aligner Therapy, Dental Ethics, and Dental Research. With years of experience in the field, I am committed to providing valuable insights and information to fellow professionals, patients, and anyone interested in the world of dentistry.